It is important to know how prostatitis is diagnosed so that you can get the treatment you need as soon as possible. Prostatitis is a condition that affects the prostate gland, and it can be difficult to diagnose since there are many different types. Your doctor will likely run several tests in order to determine if you have prostatitis and what type it is. Here are some of the most common tests used to diagnose prostatitis.
Contents
Overview of Prostatitis:
What is Prostatitis?
Prostatitis refers to four different conditions that affect the prostate gland. Two types of prostatitis are linked to urinary tract infections (UTIs). Other types are not. Men with prostatitis may have infection, inflammation and/or pain. Adult men of any age can get prostatitis.
Many men who are told they have prostatitis are misdiagnosed and actually have a different condition. There’s a lot of outdated information about prostatitis. It’s important to see a healthcare provider who is up to date on the latest prostatitis research, diagnostic tests and treatments.
There are four types of prostatitis:
- Acute bacterial prostatitis
- Chronic bacterial prostatitis
- Nonbacterial prostatitis (also called chronic pelvic pain syndrome)
- Asymptomatic inflammatory prostatitis (this type doesn’t cause symptoms)
Acute bacterial prostatitis is the least common type of prostatitis, but it’s also the most serious. It’s caused by a bacterial infection of the prostate and can lead to sepsis, a life-threatening condition.
Chronic bacterial prostatitis is a recurrent form of bacterial prostatitis. Nonbacterial prostatitis is the most common type of prostatitis. It’s often called chronic pelvic pain syndrome. Asymptomatic inflammatory prostatitis doesn’t cause symptoms, but it can be found during a medical examination for another reason.
What is the Prostate Gland?
The prostate gland is a small, walnut-shaped gland that is part of the male reproductive system. The gland sits below the bladder and in front of the rectum. The urethra (tube that carries urine and semen out of the body) runs through the center of the gland.
The prostate gland produces a fluid that makes up part of semen. The gland also helps to control urination by squeezing the urethra shut when you ejaculate.
Problems with the prostate gland are common in older men. The most common problem is an enlarged prostate, which can cause difficulty urinating. Other problems include cancer and inflammation of the prostate.
How Common Is Prostatitis?
Prostatitis is extremely common, affecting half of all men at some point in their lives. It is the most common urinary tract issue in men younger than 50 and the third most common in men over 50. More than two million men see a healthcare provider every year for prostatitis symptoms. If you are experiencing any symptoms of prostatitis, it is important to see a doctor so that you can receive the proper diagnosis and treatment.
What Are The Types Of Prostatitis?
Types of prostatitis include:
1. Acute bacterial prostatitis (category 1):
Acute bacterial prostatitis is a serious condition that requires immediate medical treatment. If you think you may have this condition, please see a doctor right away. Symptoms include fever and chills, as well as pain during urination or difficulty urinating. Acute bacterial prostatitis can be life-threatening if not treated promptly, so it is important to seek help as soon as possible. Thanks for your attention.
2. Chronic bacterial prostatitis (category 2):
Chronic bacterial prostatitis (category 2) is a condition in which bacteria become trapped in the prostate gland, causing recurrent UTIs that are difficult to treat. The most common symptom of chronic bacterial prostatitis is pelvic pain. Other symptoms may include urinary frequency and urgency, difficulty urinating, and ejaculatory pain. If left untreated, chronic bacterial prostatitis can lead to serious complications, such as bladder or kidney infection. Treatment for chronic bacterial prostatitis typically involves antibiotics. In some cases, surgery may be necessary to remove the infected tissue.
3. Chronic pelvic pain syndrome, or CPPS (category 3):
Chronic pelvic pain syndrome (CPPS) is a condition that causes chronic pain in the pelvis, perineum, and genitals. It is the most common type of prostatitis, occurring in approximately 1 out of 3 men. The exact cause of CPPS is unknown, but it is believed to be due to inflammation of the prostate gland. Treatment for CPPS typically involves medications to reduce inflammation and pain relief. In some cases, surgery may be necessary to relieve the symptoms of CPPS.
4. Asymptomatic inflammatory prostatitis (category 4):
This condition causes prostate gland inflammation but no symptoms. You may learn you have this condition after getting tests to find the cause of other problems. For example, a semen analysis for infertility may detect asymptomatic inflammatory prostatitis. This type doesn’t need treatment.
If you have asymptomatic inflammatory prostatitis, you probably won’t have any symptoms. The inflammation may be found when testing for other conditions. For example, it may be found during a semen analysis if you are being tested for fertility issues. There is no need to treat asymptomatic inflammatory prostatitis since it does not cause any symptoms.
Is Prostatitis A Sign Of Prostate Cancer?
No, prostatitis is not a sign of prostate cancer. However, the inflammation from prostatitis can sometimes raise the level of prostate-specific antigens (PSA) in blood. This is why it’s important to have further tests done to determine what’s causing your elevated PSA levels. Prostatitis itself is benign (not cancerous) and doesn’t increase your risk of developing prostate cancer. However, if you’re experiencing any symptoms of prostatitis, it’s important to see a doctor so that they can rule out any other potential causes.
What Are The Complications Of Prostatitis?
Acute bacterial prostatitis can lead to sepsis, a potentially life-threatening condition caused by widespread inflammation. Men with this form of prostatitis require immediate medical treatment.
Antibiotics, which are often used to treat prostatitis, can cause an upset stomach. Men with chronic bacterial prostatitis may need to take antibiotics frequently to control recurring infections. Some people develop antibiotic resistance, making treatment ineffective.
Asymptomatic inflammatory prostatitis can lower sperm count, affecting fertility. Complications from this type of prostatitis are rare but can include urinary tract infections and chronic pain.
Symptoms And Causes:
What Causes Prostatitis?
There are several different types of prostatitis, which can have different causes. The most common type, chronic pelvic pain syndrome (CPPS), does not have a clear cause. However, there are some potential contributors to CPPS, such as autoimmune diseases, pelvic floor muscle spasms, and stress.
The bacterial forms of prostatitis can be caused by bladder infections or stones, surgery or biopsy requiring use of a urinary catheter, prostate stones, or urinary retention (not emptying the bladder completely). UTIs may also be a cause of bacterial prostatitis.
If you are experiencing any symptoms of prostatitis, it is important to see your doctor so that the cause can be determined and appropriate treatment can be given. Treatment will vary depending on the type and cause of prostatitis.
What Are The Symptoms Of Prostatitis?
Prostatitis symptoms vary depending on the type and cause. People with asymptomatic inflammatory prostatitis don’t have any symptoms.
Men with chronic pelvic pain syndrome or chronic bacterial prostatitis may experience:
- Pain in the penis, testicles or perineum (area between the testicles and rectum). The pain may radiate to the lower back.
- Frequent urge to urinate.
- Painful urination (dysuria).
- Weak urine flow or urine stream that starts and stops.
- Painful ejaculation or pain during intercourse.
- Blood in semen (hematospermia).
- Erectile dysfunction.
- Urinary urgency (a strong need to urinate) or hesitancy (difficulty starting a stream of urine).
- Straining to urinate.
- Dribbling after urination.
- Blood in the urine or semen.
- Body aches and muscle pains.
Acute bacterial prostatitis causes a fever in addition to the above symptoms. If you experience any of these symptoms, it’s important to see a doctor so they can determine the cause and recommend treatment.
How Prostatitis Is Diagnosed?
If you think you may have prostatitis, it’s important to see your healthcare provider. They will assess your symptoms and perform a physical examination.
Less invasive tests for prostatitis may include:
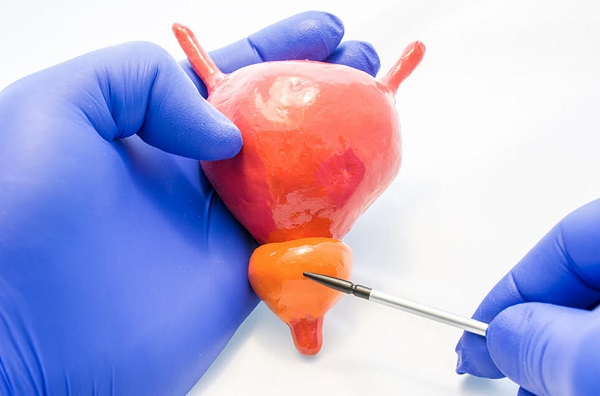
- Digital rectal exam: A digital rectal exam is a quick and easy way for your healthcare provider to check your prostate gland for any pain or swelling. The procedure involves your provider inserting a gloved, lubricated finger into the rectum in order to feel the prostate gland. This exam may include prostate massage to collect a sample of seminal fluid
- Urinalysis: A urinalysis is a test of your urine. A urine culture checks for bacteria and UTIs.
- Blood test: A blood test is often used to measure PSA levels. PSA, or prostate specific antigen, is a protein made by the prostate gland. High PSA levels may indicate prostatitis, BPH, or prostate cancer. PSA testing can be used to screen for prostate cancer, but it is not a perfect test. PSA levels can be elevated in men with prostatitis or BPH, and they can also be normal in some men who have prostate cancer. If your PSA levels are elevated, your doctor will likely order additional tests to confirm the diagnosis.
More invasive tests for prostatitis include:
- Cystoscopy: A cystoscopy can be used to look for other urinary tract problems, but it cannot diagnose prostatitis. Your provider will use a cystoscope (a pencil-sized lighted tube with a camera or viewing lens on the end) to view inside the bladder and urethra. This procedure can help rule out other possible causes of your symptoms.
- Transrectal ultrasound: Transrectal ultrasound is a imaging test that can be used to examine the prostate gland. The test involves inserting a slender probe into the rectum, which then uses sound waves to produce images of the prostate gland. This type of ultrasound can be helpful in identifying abnormalities of the prostate gland, such as abscesses or stones. Transrectal ultrasound may be recommended for men who have acute bacterial prostatitis or chronic bacterial prostatitis that does not improve with antibiotics.
Management And Treatment:
How is chronic pelvic pain syndrome (CPPS) managed or treated?
To treat chronic prostatitis/chronic pelvic pain syndrome (CPPS), your healthcare provider may use a system called UPOINT. UPOINT classifies symptoms into six categories: urinary, psychological, organ-specific, infection, neurologic/systemic, and tenderness/pain points. Your provider uses multiple treatments at the same time to treat only the symptoms you’re experiencing.
Approximately 80% of men with CPPS improve with the UPOINT system. If you have CPPS, your provider will work with you to develop a treatment plan that is tailored to your specific needs. Treatment options for CPPS include:
- Urinary: There are a number of medications that can help to improve urine flow in men with an enlarged prostate. These include tamsulosin (Flomax®) and alfuzosin (Uroxatral®), which work by relaxing the muscles around the prostate and bladder. Other medications that may be prescribed by a doctor include finasteride (Proscar®) and dutasteride (Avodart®), which can help to reduce the size of the prostate.
- Psychosocial: It is also important to manage stress levels, as this can often aggravate symptoms of an enlarged prostate. Some men find it helpful to see a counselor or therapist to talk about their anxiety, depression and other stressors. In addition, there are a number of medications that can help to relieve symptoms of anxiety and depression.
- Organ: There are also some natural supplements that may help to reduce the size of the prostate gland. Quercetin is a plant-based compound that has been shown to have anti-inflammatory properties. Bee pollen is another natural supplement that has been traditionally used to treat a variety of health conditions, including an enlarged prostate.
- Infection: Antibiotics kill infection-causing bacteria. If you have an infection, your doctor will prescribe antibiotics.
- Neurologic: Prescription pain medicines, such as amitriptyline (Elavil®) and gabapentin (Gralise®), relieve neurogenic pain. This pain can include fibromyalgia or pain that extends into the legs, arms or back. These medicines work by interfering with pain signals sent from the nerves to the brain.
- Tenderness: Pelvic floor physical therapy may include myofascial release (gentle massage to ease tension on tight pelvic floor muscles). This therapy can reduce or eliminate muscle spasms. Pelvic floor physical therapy can also help to stretch and lengthen tight muscles, which can lead to pain relief.
How are bacterial forms of prostatitis managed or treated?
Acute bacterial prostatitis is a serious condition that requires prompt treatment with antibiotics. Men with this condition may need 14 to 30 days of antibiotics, starting with IV antibiotics in the hospital. Rarely, men need surgery to drain an abscess on the prostate.
Chronic bacterial prostatitis is a more challenging condition to treat. You may need up to three months of antibiotics to sterilize the prostate. If the prostate can’t be sterilized, low-dose antibiotics can be used long term to prevent recurrences. Some men need surgery to remove prostate stones or scar tissue in the urethra. Rarely, surgeons remove part of the prostate.
If you have either type of bacterial prostatitis, it’s important to finish all of your antibiotics, even if you start feeling better. Stopping antibiotics early can allow the bacteria to multiply and cause a relapse.
FAQs of Prostatitis:
How can I prevent prostatitis?
If you are experiencing any pain in your perineum when sitting, it is important to see a healthcare provider right away. This is because prompt treatment for urinary tract infections (UTIs) may keep the infection from spreading to the prostate. Taking steps to address this problem before it leads to chronic pelvic pain syndrome can help you avoid long-term pain and discomfort.
What is the prognosis (outlook) for people who have prostatitis?
Acute bacterial prostatitis can be cured with antibiotics. These medications also ease chronic bacterial prostatitis symptoms in approximately 30% to 60% of men. Up to 80% of men with chronic pelvic pain syndrome feel better after receiving appropriate treatments for their symptoms using the UPOINT system. Men with asymptomatic inflammatory prostatitis don’t need treatment.
When should I call the doctor?
If you experience any of the following symptoms, you should call your healthcare provider:
- Blood in your urine or semen.
- Difficulty urinating.
- Frequent urination (incontinence).
- Pain during urination or intercourse.
What type of prostatitis do I have?
There are four main types of prostatitis, each with different causes and treatment options. Knowing which type you have is important in determining the best course of treatment.
What is the best treatment for this type of prostatitis?
There are several different types of prostatitis, each with its own set of symptoms and treatment options. The best way to determine the most effective treatment for your specific type of prostatitis is to work closely with your healthcare team. Together, you can create a plan that takes into account your individual symptoms, health history, and preferences.
For some types of prostatitis, such as acute bacterial prostatitis, antibiotics are the mainstay of treatment. These medications can help clear the infection and relieve symptoms. Other types of prostatitis, such as chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS), may be more difficult to treat. In these cases, a combination of lifestyle changes, medications, and complementary therapies may be recommended.
What are the treatment risks and side effects?
There are a number of risks and side effects associated with the treatment of prostatitis. These include:
- Infection: Prostatitis is a condition that is caused by bacteria, and as such, there is always the risk of infection when undergoing treatment. If the infection is not properly treated, it can spread to other parts of the body and cause serious health complications.
- Bleeding: Treatment for prostatitis often involves surgery, and there is always the risk of bleeding during or after surgery. In some cases, this bleeding can be severe and may require additional medical treatment.
- Pain: Pain is a common side effect of prostatitis treatment, especially after surgery. In some cases, this pain can be severe and may require pain medication.
- Urinary problems: Urinary problems are another common side effect of prostatitis treatment. These can include difficulty urinating, urinary incontinence, and urinary tract infections.
- Sexual problems: Sexual problems are also a possible side effect of prostatitis treatment. These can include erectile dysfunction, decreased libido, and orgasm problems.
It is important to discuss all of the potential risks and side effects of prostatitis treatment with your doctor before starting any treatment. This will help you make an informed decision about whether or not the benefits of treatment outweigh the risks.
How can I avoid getting prostatitis again?
There are a few things you can do to help prevent prostatitis from recurring:
- Drink plenty of fluids, especially water, to keep your urine diluted and flowing freely.
- Empty your bladder completely when you go to the bathroom.
- Wipe from front to back after using the toilet, to avoid spreading bacteria from your anus to your urethra.
- Avoid holding in your urine for long periods of time.
- Wear loose-fitting underwear and pants that don’t constrict your genitals.
- Avoid sitting for long periods of time without taking a break to move around.
If you have prostatitis, it’s important to finish your full course of antibiotics even if you start feeling better. Stopping antibiotics early can allow the infection to come back stronger. In some cases, prostatitis may be a chronic (long-term) condition that requires ongoing treatment.
What type of follow-up care do I need after treatment?
It is important to follow up with your doctor after treatment for prostatitis. Your doctor will likely recommend that you:
- Drink plenty of fluids
- Avoid sexually transmitted infections
- Avoid strenuous activity or lifting heavy objects
- Take pain medication as needed
- Use a heating pad on your lower abdomen or pelvis
- Follow a healthy diet and exercise regularly
- Avoid alcohol and cigarettes
If you have any questions or concerns, be sure to talk to your doctor. They can help you create a plan for managing your prostatitis and staying healthy.
Should I look out for signs of complications?
Yes, you should look out for signs of complications when you have prostatitis. Complications can include urinary retention, infection, and inflammation. If you experience any of these complications, it is important to seek medical treatment right away. Treatment for prostatitis can vary depending on the severity of the condition, but may include antibiotics, pain relievers, and warm baths. Prostatitis can be a chronic condition, so it is important to work with your doctor to develop a long-term treatment plan that is right for you.
If you have prostatitis, it is important to monitor your symptoms and watch for any signs of complications. Some common complications of prostatitis include urinary retention, infection, and inflammation. If you experience any of these complications, it is important to seek medical treatment right away. Treatment for prostatitis can vary depending on the severity of the condition, but may include antibiotics, pain relievers, and warm baths. Prostatitis can be a chronic condition, so it is important to work with your doctor to develop a long-term treatment plan that is right for you.
What prostatitis feels like?
Prostatitis is a condition that can cause a range of symptoms, including pain, difficulty urinating, and sexual dysfunction. The exact cause of prostatitis is often unclear, but it is thought to be either due to an infection or inflammation of the prostate gland. Treatment for prostatitis often focuses on relieving symptoms and may include antibiotics, pain relief medication, and lifestyle changes. In some cases, prostatitis may resolve without any treatment.
Prostatitis can cause a range of symptoms, depending on the underlying cause. The most common symptom is pain, which can be felt in the lower back, pelvis, or groin. Other symptoms may include difficulty urinating, urinary urgency and frequency, bloody urine, and sexual dysfunction.
How long prostatitis last?
Prostatitis is a condition that can cause pain and inflammation in the prostate gland. It can be acute, meaning it comes on suddenly and lasts for a short period of time, or chronic, meaning it develops over time and lasts for months or even years. In some cases, prostatitis can resolve without treatment, but in other cases, it may require medical intervention. The course of treatment will depend on the underlying cause of the condition.
Acute prostatitis typically resolves within a few weeks with antibiotics and pain relief medication. Chronic prostatitis may take longer to treat, and may require multiple rounds of antibiotics or other medications. Some men may also need to make lifestyle changes, such as increasing their fluid intake or avoiding activities that can aggravate the condition. With treatment, most men with prostatitis will see a reduction in symptoms and eventually make a full recovery.
How many prostate biopsies are enough?
The number of prostate biopsies that are needed varies from man to man. In general, the more risk factors a man has for prostate cancer, the more biopsies he may need. Some men may only need one or two biopsies, while others may require several over time. There is no set number of biopsies that all men should have, but rather it is important to discuss with your doctor how often you should be screened based on your individual risk factors.
It is important to remember that a prostate biopsy is not 100% accurate. In some cases, the biopsy may miss cancer that is present. In other cases, it may identify areas of abnormal tissue that are not cancerous. For this reason, it is important to have regular follow-up appointments with your doctor even if you have had a negative biopsy result. If you have any concerns about your risk for prostate cancer or your need for prostate biopsies, be sure to discuss them with your doctor.
How many prostate biopsies are performed each year?
In the United States, approximately 1.3 million prostate biopsies are performed each year. This number has been increasing in recent years, due to both the aging population and the availability of new, more sensitive prostate cancer screening tests. The vast majority of these biopsies are performed on men over the age of 50. African American men are at especially high risk for prostate cancer and have a higher rate of biopsy than white men.
How many prostate biopsies can you have?
You can have multiple prostate biopsies, but there is a risk of complications increasing with each procedure. The most common complication is infection, which can be serious. There is also a risk of bleeding and bruising. If you have had multiple biopsies, your doctor will closely monitor you for any potential complications.
How much prostate surgery cost?
There is no one-size-fits-all answer to this question, as the cost of prostate surgery can vary depending on a number of factors. These can include the type of surgery being performed, the experience and expertise of the surgeon, the location of the procedure, and more.
That said, it is possible to provide some general guidance on the cost of prostate surgery. For example, a basic prostatectomy (surgical removal of the prostate gland) can typically range from $5,000 to $10,000. More complex procedures, such as radical prostatectomies (which may also involve removing nearby lymph nodes), can often cost upwards of $20,000.
Of course, it’s important to keep in mind that these are just estimates – the actual cost of your surgery may be higher or lower depending on your specific situation. If you’re concerned about the cost of prostate surgery, be sure to discuss your options with your doctor or a financial advisor.
Conclusion:
Prostatitis is a general term used to describe inflammation of the prostate gland. There are several different types of prostatitis, each with it’s own set of symptoms. Because there are so many potential causes and variations in how the disease manifests, diagnosing prostatitis can be difficult. In this post, we’re going to take a look at how prostatitis is diagnosed. If you or someone you know is experiencing symptoms that could be indicative of prostatitis, read on for more information on how the condition is diagnosed.
Read more: Male Reproductive System: A Detailed Introduction